Ultimate Guide to Remote Patient Monitoring
Welcome to the CareSimple ultimate guide to remote patient monitoring (RPM), your source for all the information you need to understand this important model of healthcare delivery. From the basics through to advanced uses and the likely future, we’ll walk you through every aspect of RPM, and its context within the larger U.S. healthcare system.
Don’t forget to bookmark this page —there’s more to come, and we’ll update it as news develops, technology changes, and new reimbursement amounts are introduced.
RPG Glossary and FAQ
FAQ:
What is remote patient monitoring?
Remote patient monitoring (RPM) is a healthcare practice in which patients are monitored remotely using technology such as wearable devices, smartphones, and other digital tools. This allows healthcare providers to monitor a patient’s health status, symptoms, and other important health metrics without requiring the patient to be physically present in a clinic or hospital.
Who can benefit from remote patient monitoring?
Remote patient monitoring can be beneficial for a wide range of patients, including those with chronic conditions such as diabetes, heart disease, and respiratory disorders. It can also be useful for patients who are recovering from surgery or other medical procedures, and for patients who need regular monitoring but are unable to visit a clinic or hospital regularly.
Why is remote patient monitoring important?
Remote patient monitoring is important because it allows healthcare providers to monitor their patients more closely and provide more timely and effective care. By using RPM, healthcare providers can detect changes in a patient’s health status more quickly, which can help prevent the progression of chronic conditions and reduce the risk of complications. RPM can also help reduce the need for hospital visits and improve patients’ overall quality of life.
How does remote patient monitoring work?
Remote patient monitoring typically involves the use of wearable devices or other digital tools that allow patients to track and monitor their health status. These devices may include wearable fitness trackers, blood pressure monitors, glucose monitors, and other specialized devices. The data collected by these devices is then transmitted to the patient’s healthcare provider, who can use it to monitor the patient’s health and provide appropriate care.
What are the potential drawbacks of remote patient monitoring?
One potential drawback of remote patient monitoring is that it may require patients to purchase and use specialized equipment, which can be expensive and may not be covered by insurance. Additionally, RPM relies on patients to accurately track and report their health data, which may not always be possible or reliable. Finally, RPM may not be suitable for all patients, particularly those who are unable to use the necessary technology or who prefer in-person care.
What is the role of a healthcare provider in remote patient monitoring?
The role of a healthcare provider in remote patient monitoring is to monitor the data collected by the patient’s wearable devices or other digital tools, and to provide appropriate care based on that data. This may involve providing advice or guidance to the patient, making changes to the patient’s treatment plan, or scheduling in-person visits for further evaluation or care.
What is the role of the patient in remote patient monitoring?
The role of the patient in remote patient monitoring is to use the prescribed wearable devices or other digital tools to track and monitor their health status, and to accurately report that data to their healthcare provider. This may involve taking regular readings of their vital signs, keeping track of their symptoms, and providing other information as requested by their healthcare provider.
Is remote patient monitoring covered by insurance?
Whether or not remote patient monitoring is covered by insurance will depend on the specific policy and the type of equipment used. In some cases, insurance may cover the cost of certain wearable devices or other digital tools used for RPM, while in other cases the patient may be responsible for paying out of pocket. It is important for patients to check with their insurance provider to determine what is covered under their policy.
What are the potential long-term benefits of remote patient monitoring?
The potential long-term benefits of remote patient monitoring include improved health outcomes for patients, reduced healthcare costs, and improved patient satisfaction. By providing timely and effective care, RPM can help prevent the progression of chronic conditions and reduce the need for hospital visits and other costly medical interventions. It can also help improve patients’ overall quality of life by allowing them to manage their health more effectively and live independently for longer.
Is remote patient monitoring only available for certain conditions?
Remote patient monitoring is not limited to only certain conditions and can be used for a wide range of patients and health concerns. However, it is typically most beneficial for patients with chronic conditions or those who require regular monitoring of their health status. Examples of conditions that may be appropriate for remote patient monitoring include diabetes, heart disease, respiratory disorders, and mental health conditions.
What are some common challenges associated with remote patient monitoring?
Some common challenges associated with remote patient monitoring include the need for patients to use specialized equipment, the need for accurate and reliable data reporting, and the potential for technology-related issues. Additionally, there may be challenges related to patient adherence and engagement, as some patients may be resistant to using RPM or may not fully understand how to use the prescribed technology.
Can remote patient monitoring replace in-person visits with a healthcare provider?
Remote patient monitoring should not be seen as a replacement for in-person visits with a healthcare provider. While RPM can provide valuable information and support for patients, it should be used as part of a comprehensive care plan that includes regular in-person visits for evaluation and treatment. In-person visits are important for performing physical examinations, conducting diagnostic tests, and providing other forms of care that cannot be provided remotely.
How is patient data protected in remote patient monitoring?
Patient data is protected in remote patient monitoring through the use of secure communication channels and encrypted data storage. This ensures that patient data is not accessible to unauthorized individuals and is only accessible to the patient’s healthcare provider. Additionally, patients may be required to provide their consent before their data is collected and used for RPM, and they may be able to review and control their data through secure patient portals.
What are some examples of wearable devices used in remote patient monitoring?
Some examples of wearable devices used in remote patient monitoring include fitness trackers, blood pressure monitors, glucose monitors, and heart rate monitors. These devices may be worn on the wrist, arm, chest, or other parts of the body, and are designed to track and monitor specific health metrics. Other digital tools used for RPM may include smartphones, tablets, and other devices that can be used to collect and transmit health data.
Can remote patient monitoring be used to monitor the health of older adults or individuals with disabilities?
Yes, remote patient monitoring can be used to monitor the health of older adults and individuals with disabilities. In fact, RPM may be particularly beneficial for these populations, as it can help reduce the need for in-person visits and provide a more convenient and accessible way to track and manage health. However, it is important to consider any limitations or challenges that these individuals may face, such as difficulty using technology or limited mobility, and to provide appropriate support and accommodations as needed.
How do healthcare providers determine which remote patient monitoring technology is appropriate for a given patient?
Healthcare providers may determine which remote patient monitoring technology is appropriate for a given patient based on a number of factors, including the patient’s condition, symptoms, and overall health status. They may also consider the patient’s preferences and any limitations or challenges the patient may face, such as difficulty using technology or limited mobility. Additionally, healthcare providers may consider the cost and availability of different RPM technologies, as well as their own experience and expertise in using these technologies.
Are there any potential risks associated with remote patient monitoring?
There may be potential risks associated with remote patient monitoring, such as the risk of technology failure or data loss. Additionally, RPM may not be suitable for all patients, particularly those who are unable to use the necessary technology or who prefer in-person care. It is important for healthcare providers to carefully assess the risks and benefits of RPM for each patient, and to provide appropriate support and guidance to ensure that it is used safely and effectively.
How can patients ensure that they are getting the most out of their remote patient monitoring experience?
Patients can ensure that they are getting the most out of their remote patient monitoring experience by following the instructions and guidance provided by their healthcare provider, using the prescribed technology consistently and accurately, and actively engaging with their healthcare provider to discuss their health status and any concerns or questions they may have. Additionally, patients may benefit from seeking support from friends, family, or support groups to help them stay motivated and engaged with their RPM regimen.
How can remote patient monitoring improve the efficiency of healthcare delivery?
Remote patient monitoring can improve the efficiency of healthcare delivery by allowing healthcare providers to monitor their patients more closely and provide timely and effective care. By using RPM, healthcare providers can detect changes in a patient’s health status more quickly and respond with appropriate interventions, which can help prevent the progression of chronic conditions and reduce the need for hospital visits and other costly medical interventions. Additionally, RPM can help reduce the burden on healthcare providers by allowing them to manage more patients without requiring additional staff or resources.
What is the future of remote patient monitoring?
The future of remote patient monitoring is likely to involve the continued development and refinement of technology, as well as an increasing emphasis on integration with other aspects of healthcare delivery. For example, RPM may become more closely integrated with electronic medical records and other digital tools, allowing for more seamless and efficient care. Additionally, there may be a growing focus on using RPM to support the management of chronic conditions and other complex health concerns, as well as to improve the overall quality and accessibility of healthcare.
Glossary:
Patients, care, healthcare.
Remote Patient Monitoring, chronic conditions, pulse oximeter, blood, disease, condition
Vital signs, medical devices, healthcare organizations, blood pressure cuff, chronic diseases, practices. Visits, difference, review, remote patient monitoring programs.
Remote patient monitoring devices, center, Remote Monitoring, RPM devices.
RPM program, heart rate, remote patient monitoring services.
COVID-19 patients, readmission, person care, patient care, mortality, healthcare providers
Quality of life lives, survey, heart disease, clinical practice, population, emergency room visits, person visits, analysis.
Systems, wide range, skilled nursing facility, benefits of RPM, providers for assessment, remote monitoring devices, patient health, hospital readmission, chronic care management.
BEAT-HF, Healthcare IT News, qualified healthcare professional, blood pressure.
Blood glucose levels, blood pressure readings, pulmonary disease, and emergency department visits.
Acute conditions, systematic review, content, Kaiser Permanente, chronic patients, effects among patients.
Readmissions among patients, patient home monitoring program, ambulatory patients, broad patient eligibility criteria, decompensation in patients.
Hospitalizations in Cancer Patients, Intervention patients.
Remote patient management, remote patient telemonitoring.
30-day all-cause readmission, readmission with receipt, 30-day readmission, the focus of readmission reduction.
Models for readmission, readmission reduction efforts, all-cause readmission.
180-d readmission analyses, readmission after hospitalization, secondary readmission outcome measures, usual care participants, Care Innovations, care modality, care transition management, monitoring with care transition.
BEAT-HF intervention, BEAT-HF project managers, BEAT-HF study, BEAT-HF enrolment nurses.
BEAT-HF funding, BEAT-HF post-discharge intervention nurses, BEAT-HF research staff.
BEAT-HF trial, 180-day all-cause mortality, 30-day all-cause mortality, mortality with receipt.
180-day mortality, 30-day mortality, mortality analyses, 30-day mortality findings, healthcare team, blood sugar levels, life score, life improvements.
Life Inc, life outcomes, 180-day survey respondents, characteristics from survey respondents, survey nonrespondents.
Survey response rates, medical centers, telephone call center intervention.
Telephone call center nurses, actual practice, physician practices, broad population.
Population Health Research Institute, population of patients hospitalized.
Hospital death differences, Non-significant differences, adjusted analysis.
Statistical analysis, review of deaths suggest, intellectual content.
Supplemental content, hemodynamic monitoring systems, tele monitoring system vendor.
Covid-19, understanding, rpm, patients, public health, telemedicine, digital health, payment, ama.
Patient, American medical association, technology, CPT, medication adherence, patient monitoring.
White papers, remote patient monitoring, medicare, inbox, reimbursement, pandemic
Copd, remote physiologic monitoring, hospital, safety, health, applications, telehealth.
Wearables, definition, amazon, cost, organization, calculator, door, modality.
Market, technologies, app, medicine, learning, diabetes, science, resource, table of contents, hospice, fee, clinic.
Hypertension, medical education, chronic care management, medical service, stress, video, cardiovascular risk, data, physician, physicians, hospitalizations, vaccine, pulmonology, research, blog, length of stay, clinical evidence.
Policies, emergency, policy, healthcare industry, California, blood pressure cuff.
Covid-19 public health, burnout, peak expiratory flow, cureatr, audits.
Massachusetts, Alaska, Connecticut, webinars, readmissions, eCommerce, retail, financial services, georgia, protocols, health care.
New york, Puerto Rico, bivalent, medical schools, loans, parental leave, Illinois, Missouri, cybersecurity, health sector, free content, hhs, Ohio.
Endocrinology, hrs, cardiac, medical student, Iowa, North Carolina.
Kentucky, Delaware, Arizona, health service, mayo clinic health system, healthcare, preventive care, languages, Hawaii, Orion health, residency, mainstream.
Indiana, Oregon, Alabama, training, med student, Oklahoma, New Hampshire, Louisiana, Kansas, news, pandemics.
Email, triage, state, palliative care, Arkansas, activity trackers, newsletter, intelligence, stethoscope, Montana, Nebraska, Idaho, Nevada.
North Dakota, New Mexico, company, Wisconsin, statistics, sales, mobile.
Pennsylvania, Colorado, Maryland, population health, inpatient, Florida, New Jersey, education, privacy policy.
Health systems, pulse oximeter, ECG, Maine, download, Mississippi, cardiology, compliance, Bluetooth, well-being, stakeholders.
Advocacy, password, Michigan, immunization, sound, dashboard, knowledge, library, quality of life, webinar, menu.
Best practices, growing, it’s, personal, short, multi, ones, vendor, here’s, develop, as remote.
Telehealth policy, ask, coverage, monitoring services, covid, via rpm, playbook, grow, as rpm.
Connecting, would, issue, issues, window, often, ama, s growing, connected health policy.
Between, organizations, levels, stories, FDA, organ, advance, symptoms, science, around, multiple, apis, early, virtual visits.
Table of Contents
What Is Remote Patient Monitoring?
Is Remote Patient Monitoring the Same Thing as Telehealth?
A Brief History of Telehealth and RPM
The RPM Model, as Defined by CPT Reimbursement Codes
What Technology Is Used to Deliver RPM?
Quick Guide to RPM Devices: RPM Blood Pressure Monitor
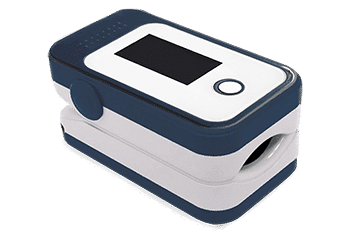
Quick Guide to RPM Devices: RPM Pulse Oximeter
Quick Guide to RPM Devices: RPM Weight Scale
Quick Guide to RPM Devices: RPM Spirometer
Quick Guide to RPM Devices: RPM Glucometer
The Benefits of Remote Patient Monitoring
How Does Remote Patient Monitoring Benefit Patients?
How Does Remote Patient Monitoring Benefit Providers?
How Does Remote Patient Monitoring Benefit Payers?
RPM Cost Factors: Facility Type
RPM Cost Factors: Population Type
RPM Cost Factors: Workforce Adjustments
RPM Cost Factors: Type of Devices Needed (and How Many)
RPM Cost Factors: Type of Software
RPM Cost Factors: Analytics and Reporting
Other Care Management Models that Use RPM
How RPM Supports Population Health Management
How RPM Supports Hospital-at-Home (HaH) Programs
Looking for More Info or Guidance on Remote Patient Monitoring?
The Basics of Remote Patient Monitoring
What is remote patient monitoring, and why is it so important to patient care today?
And is it the same thing as telehealth? Let’s start at the start.
What Is Remote Patient Monitoring?
Remote patient monitoring (RPM) is a model of care delivery that in which patient information is tracked, monitored and/or managed on a remote (or virtual) basis. In general, RPM lets patients stay at home while receiving attentive, high-quality care for chronic illnesses, serious injury or other conditions.
Using remote patient monitoring, doctors and other practitioners can closely monitor the vital signs and other essential data like heart rate and blood pressure of certain patients while they’re at home, with no need for lengthy and expensive hospital stays. RPM care also includes regular check-ins, usually also carried out remotely (via phone or a video chat, for instance).
In the past, RPM was most often used to provide care in the home for people with chronic conditions, including severe respiratory conditions, heart and kidney disease, diabetes, cancer, and others, as well as those recovering from serious injury. Today, it has expanded to cover many other aspects of patient care, particularly since the COVID-19 pandemic has accelerated the demand for at-home care.


Is Remote Patient Monitoring the Same Thing as Telehealth?
In a larger context, RPM is a type of telehealth. Telehealth (or telemedicine, as it’s often called) is a term describing healthcare that uses technology to treat patients “across distance,” as the U.S. Centers for Medicare & Medicaid Services (CMS) defines it. “Across distance” means remotely — in other words, the patient and doctor or care team in different physical locations (although not necessarily all the time).
In addition to being a standalone model of care management, the technology that underlies RPM is also used within other care management models. These include chronic care management (CCM), transitional care management (TCM), principal care management (PCM) and other, each of which integrates a variety of RPM devices to provide at-home care for high-risk patients.
Read more about the different types of care management models that use RPM here
A Brief History of Telehealth and RPM
What is remote therapeutic monitoring? Take a deeper dive here
Part 2
How RPM Helps Deliver Patient Care
RPM is most often used to provide care for people with chronic conditions. This including COPD or other severe respiratory conditions, heart disease, kidney disease, cancer, stroke, diabetes, Alzheimer’s disease, influenza and pneumonia, and septicemia, among many others.
As with transitional care management and principal care management, the primary goal of an RPM program is to keep patients with these conditions as healthy as possible, without having to be readmitted to a hospital.
The RPM Model, as Defined by CPT Reimbursement Codes
The CPT codes for RPM offer doctors and healthcare providers reimbursement options for delivering care, as well as a predefined path for delivering that care. Although the details of the reimbursement codes change each year, the basic structure is as follows:
CPT code
99453
CPT code
99454
CPT code
99457
CPT code
99458
CPT code
There are more details to each of these codes, of course.
To read more, and to see a list of current reimbursement amounts, check out our guide to RPM codes in 2022.
What Technology Is Used to Deliver RPM?
Remote patient monitoring is possible thanks to recent advances in technology that allow efficient, seamless, and secure at-home care. Two types of technology form the basis of remote patient monitoring: virtual communication and remote medical devices.
First of all, virtual communication tools are necessary to allow caregivers to speak with patients on a regular basis. This includes the monthly check-ins that are the basis of the CPT codes for reimbursement. And, while these can certainly be delivered using new technology like videoconferencing apps (such as Zoom), in some cases it can also be delivered via telephone. Check the CPT codes for specific details.
Secondly, remote medical devices are essential for remote patient monitoring. The most common RPM devices are used to monitor vital signs, like blood pressure monitors, blood glucometers and pulse oximeters. Other RPM devices like weight scales and spirometers capture additional patient data that’s also vital to care.
Many of these RPM devices can also be used in other types of patient care. For instance, a remote blood pressure monitor is essential for chronic care management programs, while a remote spirometer is of use to providers implementing remote therapeutic programs. And the best of these devices let patients upload their information into a clinical portal and EHR/EMR in near real-time.
Quick Guide to RPM Devices: RPM Blood Pressure Monitor
A remote BP monitor tracks a patient’s blood pressure while they’re at home. Equipped with that patient data, doctors and care teams can more readily monitor events such as a morning blood pressure surge, and can more frequently check the patient’s condition to make timelier, better-informed decisions. This is especially vital for people with chronic heart conditions or hypertension.

Quick Guide to RPM Devices: RPM Pulse Oximeter
A remote pulse oximeter is designed to remotely monitor both heart rate and blood oxygen levels, which are both critical indicators for patients with chronic diseases like heart failure, lung cancer, asthma, and chronic obstructive pulmonary disease (COPD). Read more about RPM pulse oximeters.
Quick Guide to RPM Devices: RPM Weight Scale
An RPM weight scale offers a fast, easy and accurate way to remotely measure body weight without an in-person office visit. Regular weight readings can give a clinical team faster access to information that’s essential for care management. Sudden weight gain or other changes can be a red alert for certain chronic conditions (particularly heart conditions), offering opportunities for earlier intervention.

Quick Guide to RPM Devices: RPM Spirometer
RPM spirometers provide a fast and easy way to measure forced expiratory volume (FEV) and other data concerning a patient’s pulmonary (lung) function. Helpful for physicians and care providers who are managing patients with chronic conditions like COPD and congestive heart failure (CHF), remote spirometers can also be used for reimbursement for RTM care in some instances.

Quick Guide to RPM Devices: RPM Glucometer
A remote patient monitoring glucometer, or blood glucose meter, is used to provide information on a patient’s blood glucose levels — a critical health indicator for diabetic and pre-diabetic patients. An easier, more convenient way to monitor blood sugar levels means patients are better equipped to follow doctor recommendations, while giving providers better info to make treatment adjustments.

The Benefits of Remote Patient Monitoring
How Does Remote Patient Monitoring Benefit Patients?
Perhaps more than any other group, patients have embraced RPM as a means of comfortably receiving care at home. Receiving treatment in the comfort of home, surrounded by loved ones, helps offer comfort and convenience, as well as a more effective way to engage with treatment.
Not only do most people of all ages have some kind of mobile device, but many millions also regularly engage in self-care activities with step monitors and other popular apps. So, what was once a barrier to telehealth, computer literacy, is now a boon, with rates today at all-time highs today, even among seniors. (An AARP study released in 2020 found that 77% of older Americans use a smartphone.)
To better promote this comfort and convenience, the best platforms for remote patient monitoring include interface options that are easy and intuitive for patients to use. Using a browser website or a smartphone app, they can keep tabs on the details of their own care, every day. For some patients, that creates enthusiasm and engagement that were difficult to achieve with more traditional care models.
The 24/7 monitoring offered by RPM can also be a source of comfort for patients worried about their condition. For those who are already engaged with their care regimen, one of the biggest benefits of remote patient monitoring is the chance to stay in contact with doctors and caregivers about critical concerns at all times
And because it’s designed to be used across distances, RPM can particularly benefit patients who live in remote and rural areas, and therefore may not have access to the care that other people do.
And finally, RPM often lets patients receive high-level treatment at a much lower expense than traditional care, which often helps alleviate financial worries — a top concern for many patients today. The new CMS codes for remote patient monitoring and RPM-adjacent care models help ensure that this critical part of chronic care is covered by insurance (as much as 80%, after deductible).
By allowing for more at-home care, and fewer trips to the clinic or hospital, remote patient monitoring programs also offer patients other perks like less money spent on gas and time wasted traveling. And many patients are also acutely aware of the potential financial consequences of a hospital or emergency room visit, giving added appeal to the higher quality of care made possible with RPM.
There’s more, too:
Check out our list of 10 key benefits that RPM offers patients.
How Does Remote Patient Monitoring Benefit Providers?
Enhanced comfort and convenience for patients is a benefit for providers, too, offering an effective way to enhance the patient experience that’s currently top of mind for so many leaders. Greater patient acceptance can help drive engagement and adherence to a medication regimen. It can also contribute to satisfaction and overall patient health outcomes — the ultimate goal of any model of patient care.
With 24/7 monitoring, RPM also offers providers a valuable source of more detailed data than has ever been available before. This helps provide a better understanding of each patient’s condition at any given time — a critical factor in treating chronic care patients. This kind of close watching also helps prevent escalations in the patient’s condition, which can contribute to improved outcomes.
On top of that, partnering with a leading RPM platform provider means also getting access to expert guidance on how to use all that data. Advanced data analysis and reporting tools, which can be integrated into an organization’s EHR system, can quickly manage and leverage huge amounts of data to better manage patients, populations, outcomes, even workforce concerns like scheduling and planning.
RPM systems helps nurture the patient/provider relationship by offering a greater ability for communication. And given the stresses and challenges related to chronic care, that bond can be not only a source of comfort for patients, but also a better way of engaging them in their care regimen, boosting the potential for positive patient outcomes in the process.
How Does Remote Patient Monitoring Benefit Payers?
The improved data and 24/7 monitoring that helps doctors provide better care also directly benefits payers seeking to reduce claims for readmissions and escalations and other events. It also helps prevent escalations, which can contribute to improved outcomes, offering the potential to save organizations significant expenses with fewer re-hospitalizations (and the CMS penalties that can go along with them).
According to the U.S. Centers for Disease Control and Prevention (CDC), 90% of the $3.8 trillion spent each year on healthcare in the U.S. goes toward people with chronic and mental health conditions.
Correspondingly, the CDC’s website calls for reducing these costs by better preventing chronic diseases, or better managing symptoms “when prevention is not possible.”
To that end, CMS has introduced a number of ways to enable providers to provide more effective, patient-focused care for chronic illness, including the reimbursement for remote patient monitoring. By helping prevent re-admissions and escalation, RPM also helps the industry as a whole move toward value-based care, which is a benefit to everyone in the care continuum.
Estimating the Costs of Remote Patient Monitoring
RPM Cost Factors: Facility Type
What type of facility will be implementing the solution? Because it’s designed to treat patients at home, RPM can be administered by a wide variety of providers, from hospitals to post-acute facilities, and pretty much every one in between. The type of facility, and to what extent the technology is integrated, will affect the size of the implementation and subsequent cost, both in terms of initial setup and long-term financial returns.
RPM Cost Factor: Patient Population Type
Pilot programs give organizations a good idea of what to expect when scaling the program to a larger population, in terms of cost as well as outcomes. It’s also important to remember in these calculations that efficiencies often expand with wider use, further increasing the value over time. In addition, staff will become better at providing RPM services as use grows, further reducing operational costs.
RPM Cost Factor: Workforce Adjustments
Another major factor in the cost of an RPM program is whether an organization’s current staff has the skills to deliver remote care. Does your facility have any telehealth programs currently in place, for instance? Or will this be new territory for your workers? Do you have any professionals on staff who specialize in remote care — and if not, how much training will be needed?
Although many RPM partners offer employee training, facilities that implement an RPM program on a piecemeal basis may have to cover this expense on their own. An honest assessment of a facility’s true level of preparedness will help leaders understand what investments will be needed, whether in group training or access to specific CE classes around telehealth and remote care.
RPM Cost Factors: Type of Devices Needed (and How Many)
Estimating the number of RPM devices you’ll need for a specific population can be another effective way to understand the overall cost of remote patient monitoring to your organization in advance. And this is a fairly simple matter of measuring the specific needs of each patient in your pilot program.
As noted above, RPM is based on the use of a variety of remote medical devices. Which of these specific devices you need — and how many — will depend on the patients. If your pilot program is patients with COPD, for instance, or hypertension, different devices will be needed. And it should be noted that choosing devices with advanced capabilities like seamless and secure EHR transmission can help further improve a program’s chance of success, which can translate to financial ROI.
RPM Cost Factors: Type of Software
In addition to devices, RPM requires the use of software to sync up all its components into a workable, fully functional solution. There are a few options here, from one-time purchases to subscription-based services to fully integrated partners. The first requires a significant up-front payment, and continuous investments in renewals and upkeep. The others offer RPM software as a package, with no additional fees for implementation, and no added cost for security patches or scaling up to include new patients.
Investing in higher-grade RPM software could make a big difference as to whether a program is successful, while the use of lower-cost solutions could deflate the program’s overall value by requiring staff to spend long hours manually entering or trying to analyze badly organized data, for instance.
RPM Cost Factors: Analytics and Reporting
To further defray the cost of a remote patient monitoring program, leaders should look for the inclusion of an integrated program of analytics and reporting. This can help ensure continuous improvement through regular analysis of key metrics and data, which can help organization get the maximum value for a program, lowering overall costs in the long run.
For busy leaders, the information provided by analytics could help drive better-informed decisions that affect the quality of care of entire populations, thus deriving even more value from the program. So, it’s worth making the extra investment in an analytics and reporting option at an early stage — or partnering with a provider of customizable RPM solutions offering built-in tools for just this purpose.
Beyond Standalone Care: Other Care Management Models that Use RPM
“RPM today is still in its very beginning, despite all the years and sweat we’ve devoted into it,” as CareSimple CEO Michel Nadeau has explained. “But RPM is getting entrenched into a diverse set of clinical workflows, ready to be prescribed by physicians for their patients.”
In other words, as essential as it has become in delivering quality care for at-risk patients, RPM also plays an important role in supporting a number of other care management models. From post-discharge care and hospital-at-home (HaH) programs to digital therapeutics and population health management services like chronic care management (CCM), an effective RPM platform can also drive many other beneficial care management programs for healthcare providers.
How RPM Supports Population Health Management
Population health management has become central to care delivery, offering a more effective means for treating entire patient populations. By emphasizing specific outcomes, measurements and standards of accountability among patient segments, population health management can help providers improve outcomes with more specific data, save money through streamlining, among other benefits.
By enabling the regular collection, transmission and analysis of patients’ vital signs and other important physiologic data, RPM serves as the foundation for many CCM programs. In addition to devices, RPM delivers the built-in analytical power needed to distinguish and monitor other population health segments. You can read more about how RPM powers population health management solutions here.
How is RPM Different from Chronic Care Management (CCM)?
Closely associated with the treatment of chronic care, RPM can be easily mistaken for chronic care management. But as reimbursement models for patient care, there is a difference between the two — and, in fact, many providers receive reimbursement by “coupling” both models.
“CCM patients already benefit from care coordination,” as we explained in our white paper on using RPM for population health management. “These patients have therefore provided their consent for the program and are assigned to a care manager, and all have been diagnosed with two or more chronic conditions. They are all candidates for RPM as a complementary program.
“In many physician groups, patients are often managed by the same care manager. This means that simply requesting a verbal consent is often all that’s required to add the patient.”
Strictly speaking, patients must have at least two chronic conditions to qualify for CCM. The idea is to closely monitor their care and promote engagement to help them avoid readmissions and re-hospitalizations, as well as the development of comorbidities or other deterioration. You can find more details, along with the most recent codes for chronic care management (CCM), here.
How RPM Supports Post-Discharge Care
In addition to the strictly defined care parameters for CCM, RPM technology is also frequently used to treat high-risk patients in other contexts. For instance, its ability to monitor the vital signs and other important patient data gives doctors and care teams the power to better manage patients during the critical period when they’ve been discharged from acute care.
Post-discharge care of this type is delivered in two phases. Transitional care management (TCM) reimburses billing practitioners for treating patients with a complex medical condition during their 30-day post-discharge period. And principal care management (PCM) covers the reimbursement of such high-risk patients during the subsequent period, from three to twelve months in total. You can read more about PCM here, and learn more about TCM here.
How RPM Supports Hospital-at-Home (HaH) Programs
Hospital-at-home (HaH) is a type of care management model that leverages remote patient monitoring to deliver hospital-level care in a patient’s home or place of residence. In addition to promoting engagement and outcomes, HaH can also be a valuable tool in freeing up bed capacity and reducing the risk of in-hospital infection.
Like CCM, HaH is often deployed with patients suffering from serious injury or a chronic condition. Also like CCM, it can leverage RPM technology for the better monitoring of those patients, as well as the ability to offer doctors and care teams better, more timely data — and much more of it. You can read more about how RPM drives hospital-at-home programs here.
How RPM Supports Digital therapeutics
RPM solutions are also becoming critical to the newest of these models, digital therapeutics. Leveraging both telehealth and mHealth software, tools and applications to offer “a new category of medical interventions,” as Xtelligent Healthcare Media describes it, digital therapeutics can be used for chronic conditions and serious injuries, as well as a diverse range of other treatments.
Although many digital therapeutics are in their early stages, experts predict rapid growth. And for many of its potential applications — musculoskeletal (MSK) treatment for low back pain, and cognitive care relating to substance abuse, attention-deficit disorders and hyperactivity, for instance — remote patient monitoring is poised to play a major role.
Looking for More Info or Guidance on Remote Patient Monitoring?
Looking for more details on how CareSimple can help your organization better understand remote patient monitoring, or get help implementing an effective RPM program? Contact us here to connect with a CareSimple RPM specialist.
