The Centers for Medicare & Medicaid Services recently announced the ACCESS (Advancing Chronic Care with Effective, Scalable Solutions) Model, a groundbreaking 10-year voluntary payment demonstration that represents a significant shift in how Medicare pays for chronic disease management. Set to launch on July 1, 2026, the model focuses on conditions affecting more than two-thirds of Medicare beneficiaries, including high blood pressure, diabetes, chronic musculoskeletal pain, depression, and anxiety. Rather than paying for specific services or visits, ACCESS introduces an innovative Outcome-Aligned Payment (OAP) approach that rewards participating organizations for achieving measurable health outcomes, such as helping a patient with hypertension lower their blood pressure by 10 mmHg. This outcome-based structure gives clinicians flexibility to leverage digital health tools, remote monitoring technologies, and other modern care delivery methods without being constrained by traditional Medicare coverage limitations.
The missing piece in chronic care isn’t a new program — it’s what happens after RPM works.
Every health system running a successful Remote Patient Monitoring (RPM) program at scale eventually faces the same question: what do you do with patients who’ve been brought under control?
It’s not that these patients immediately fall off a cliff. Most do well for months, even a year or more. But without a structured, low-touch way to keep them engaged, many gradually drift back into old habits. Medications get skipped. Diet slips. And when they eventually resurface in a clinical setting, they’ve lost the gains that RPM helped them achieve. The problem isn’t that RPM doesn’t work — it’s that there’s been no financially sustainable way to maintain what it accomplished.
That’s the gap we’ve been discussing with our provider customers. And through those conversations, an idea has taken shape: the CMS ACCESS Model may be the ideal graduation path for patients who’ve been stabilized through RPM.
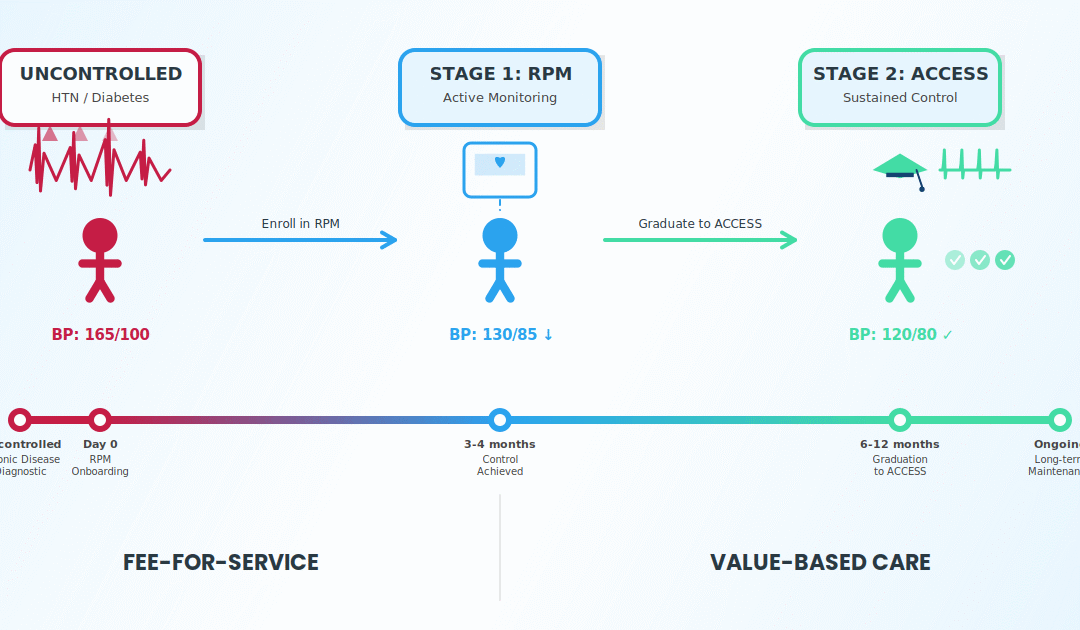
ACCESS wasn’t specifically designed as an RPM graduation pathway. But working closely with our provider customers, it became clear that it fills that role remarkably well. Here’s the two-stage model that’s emerging:
Stage 1 — Device-Based RPM
Patients with uncontrolled hypertension, diabetes, or CKD are enrolled in traditional RPM using cellular-connected devices. Daily readings, clinical interventions, and treatment adjustments bring conditions under control. Providers bill under the strengthened 2026 CPT codes with improved reimbursement rates.
Stage 2 — ACCESS Graduation
Once stabilized, patients transition into the ACCESS Model. Technology-supported care continues — telehealth check-ins, asynchronous monitoring, app-based engagement, periodic assessments — but without daily device dependency. The RPM cellular device lifecycle is extended. Payment is tied to sustaining outcomes over the long term.
This creates something that hasn’t existed before in fee-for-service Medicare: a sustainable, low-touch program that keeps stabilized patients under control while remaining financially viable for the provider organization.
Why Starting Small with Hypertension and Diabetes Makes Sense
The ACCESS Model’s clinical tracks map directly onto the conditions RPM programs manage daily. The early Cardio-Kidney-Metabolic (eCKM) track covers hypertension, dyslipidemia, obesity, and prediabetes. The Cardio-Kidney-Metabolic (CKM) track covers diabetes, CKD, and cardiovascular disease.
From the conversations we’re having in the field, hypertension and diabetes may be the first ACCESS pilot programs in 2026. The logic is straightforward: these are conditions where RPM has already demonstrated clinical impact at scale, where outcome measurement is well-defined (blood pressure targets, HbA1c levels), and where the graduation model makes immediate clinical sense.
The key constraint remains the FFS trade-off. Enrolling a patient in ACCESS means forgoing traditional fee-for-service billing for that patient. Without published OAP amounts, committing large populations carries real financial risk. Starting with a defined cohort of already-stabilized RPM patients — say, those who’ve maintained blood pressure control for 6-12 months — is the pragmatic path. It validates the graduation workflow, extends the value of devices already deployed, and positions your organization to scale once the economics are confirmed.
What This Means for the Technology Stack
The ACCESS Model requires FHIR-based API reporting, electronic care coordination with referring providers, and individual-level clinical outcome tracking. ATAAction’s recommendation to automate documentation through existing EHR workflows underscores a point we’ve been making to our customers: this isn’t a documentation exercise — it’s a technology requirement.
At CareSimple, we’re already working collaboratively with our provider customers to prepare. This means adapting our platform to automate outcome reporting, streamline the transition from device-based RPM to ACCESS-model care, and ensure the entire patient journey — from initial device enrollment through long-term outcome management — runs through a single integrated infrastructure.
The organizations that will thrive in ACCESS are those whose technology can support both stages seamlessly.
The Bottom Line
RPM brings patients under control. ACCESS can keep them there.
RPM brings patients under control. ACCESS can keep them there. Together, they create the first truly sustainable chronic care lifecycle in fee-for-service Medicare.
The application window is open until April 1 for the early movers that want to start their ACCESS program in the first window starting July 1, 2026. Interest levels and commitments for Applications and eventual execution of a Participation Agreement will depend on several yet-to-be announced details of the program. These include the annual payment rates per patient per track, the clinical outcomes goals for initial improvement and maintenance periods. The industry is actively shaping the details that will determine whether this model delivers on its promise.
The question for every health system running an RPM program today: will you be ready to graduate your first patients when it does?
Virtual Care Partnership
CareSimple provides the full-stack RPM infrastructure — cellular-connected devices, logistics, clinical workflows, EHR integration, and patient engagement — with the Collaborative Services that health systems need to build and scale RPM-empowered Virtual Care programs.
To learn how you can prepare for the ACCESS Model,
contact us at [email protected].