What is Remote Patient Monitoring?

It is estimated that 30 million U.S. patients will use remote patient monitoring (RPM) tools by 2024, and demand for the technology from health systems and health plans continues to grow. As RPM gains in popularity and demonstrates positive health outcomes, which can benefit public health, we thought it might be helpful to explain what it is exactly, how it works and the benefits it provides to both patients and providers that makes this new member of virtual care delivery systems increasingly sought-after.
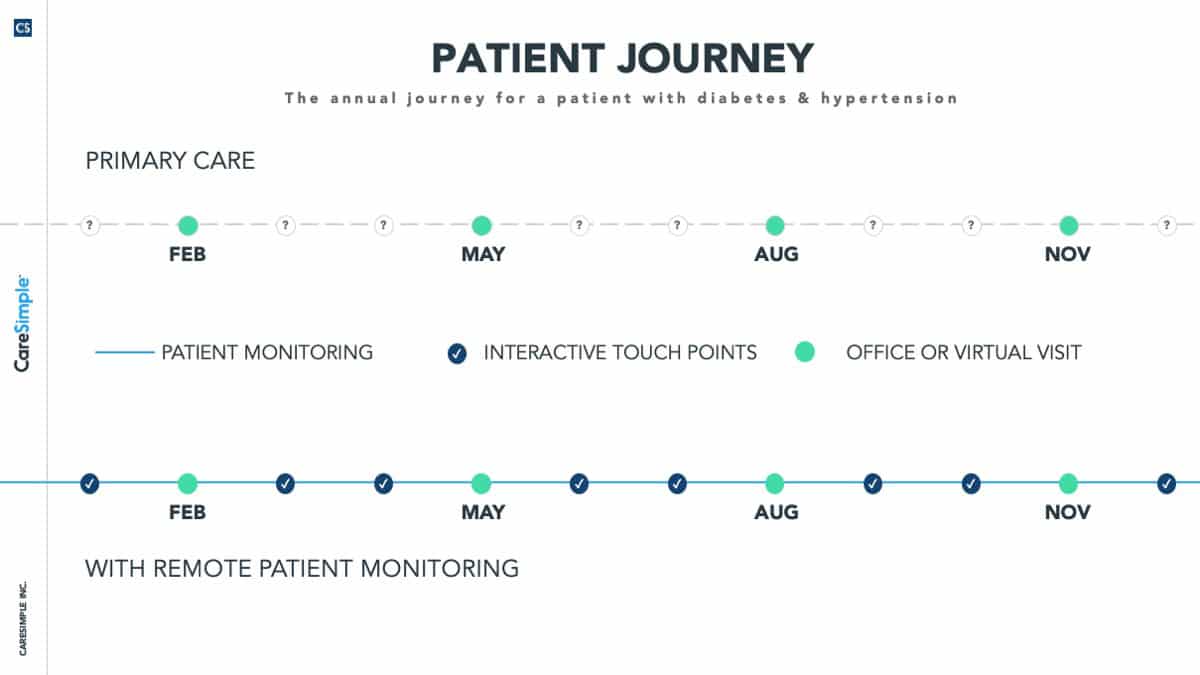
RPM is a digital health technology offering that enables the monitoring and collection of patients’ physiologic measures outside of a traditional healthcare environment, such as at a patient’s home or office. Care managers use dashboards, clinical alerts and secure messaging to deliver remote care services to patients, and patients then generate their own health data as prescribed by their care plan using monitoring devices such as blood pressure cuffs, body scales, heart rate and pulse oximetry monitors, blood glucose monitors, spirometers and mobile apps. Through 4G-enabled medical devices, the vital signs are sent electronically with ease over cellular networks directly to the physician’s office for review. RPM also incorporates the data processing, secured storage and analysis that occurs in between data collection and reporting.