Analysis performed by CareSimple with the collaboration of AI Agent:

The 2026 Medicare Physician Fee Schedule (PFS) Proposed Rule introduces key updates that expand reimbursement for Remote Patient Monitoring (RPM). Most notably, new CPT codes will allow billing for shorter monitoring periods and shorter clinical interaction time – scenarios that previously weren’t reimbursable. This increased flexibility means providers using CareSimple’s RPM platform can get paid for partial-month data and brief check-ins, enabling wider patient enrollment and recapturing revenue that was often lost under older rules. However, with greater flexibility comes greater oversight: regulators warn that these changes could be vulnerable to abuse (e.g. billing with minimal data), so compliance and careful program management will be crucial 1. Below is an executive summary of the changes and what they mean for CareSimple customers.
Key Changes in the 2026 Proposed Rule for RPM
The proposed rule delivers long-awaited flexibility in RPM billing. Three main code changes are of interest:
- 2 new RPM codes 99XX4 & 99XX5
- 3 new RTM codes 98XX4, 98XX5 & 98XX7
New Short-Duration RPM Device Code (CPT 99XX4)
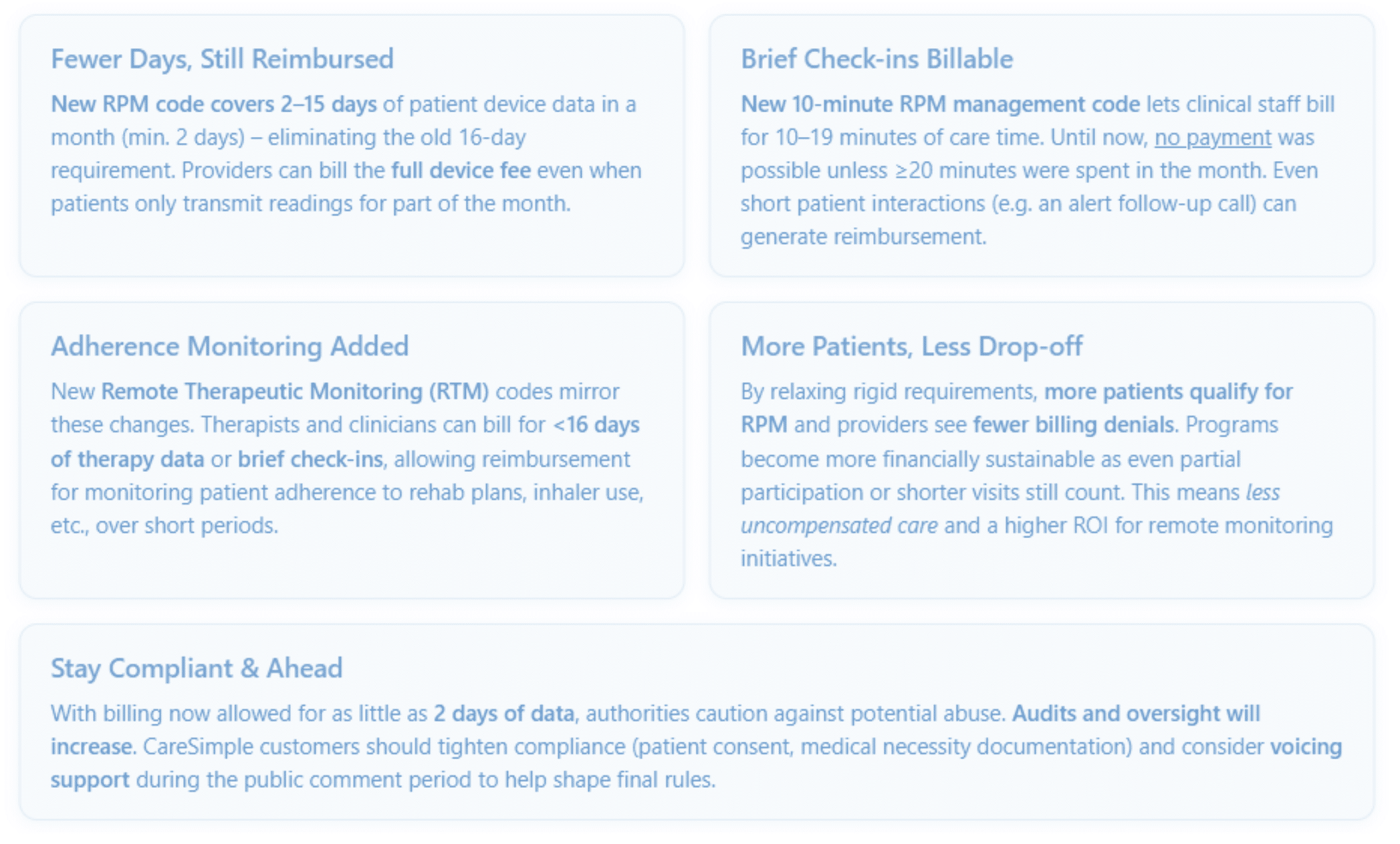
Medicare proposes a code to cover cases with fewer than 16 days of device readings in a 30-day period (minimum 2 days) 1. Under current policy, CPT 99454 (the monthly device supply & data transmission fee) requires ≥16 days of readings, so any month with only 15 or fewer days of data is not billable 1. This new code removes that all-or-nothing barrier. Providers may bill 99XX4 at the same rate as 99454, allowing reimbursement even if patients use the device intermittently or the 16 days of readings are not clinically relevant.
This change is especially useful for:
- Short-term monitoring needs (e.g. post-discharge recovery, titration of a new medication) where 16 days of data isn’t clinically necessary 1.
- Partial adherence cases – for instance, if a patient only manages 10 days of readings due to holidays or illness, the work invested in those 10 days isn’t financially wasted.
- Intermittent monitoring scenarios, like checking in on a chronic condition a few days each month.
By acknowledging clinical value in 2+ days of data, CMS is aligning payment with real-world RPM use cases.
New 10-Minute RPM Management Code (CPT 99XX5)
Currently, RPM care management (code 99457) can only be billed after ≥20 minutes spent in a month on activities like data review, patient coaching, or care coordination. If 15 minutes were spent, no payment could be claimed. The proposal introduces CPT 99XX5 to cover 10–19 minutes of RPM management time. This effectively splits the time requirement into two tiers:
- 99XX5 for the first 10-minute increment of clinical staff/physician time.
- 99457 for ≥20 minutes (the original threshold) for the first full block, with 99458 for each additional 20 min.
CMS proposes ~half the reimbursement rate for 99XX5 compared to a full 20-minute 99457, since 10 minutes is about half the work RVU. Even so, this is a welcome change: it means even brief but important check-ins are billable. For example, if a nurse spends 10 minutes in a month responding to an alert and adjusting a care plan, that time now generates revenue where before it would not. This lowers the bar for RPM programs to show financial returns, as every meaningful touchpoint counts.
Information below should not be indented here as it is separate from above.
- Expanded Remote Therapeutic Monitoring (RTM) Codes: CMS is similarly adding flexibility to RTM (which tracks patient-reported data and adherence, often used by physical therapists, respiratory therapists, etc.). New codes include:
- 98XX4 and 98XX5: RTM device supply for 2-15 days of data (for musculoskeletal and respiratory monitoring, respectively).
- 98XX7: RTM management services for 10–19 minutes of time.
These mirror the RPM changes and acknowledge that therapeutic adherence monitoring (e.g. exercise logging, symptom reporting) can have value even if done for a shorter duration or with only a brief check-in. It broadens reimbursement for digital therapeutic programs, meaning providers can get paid for coaching patients on rehab exercises or asthma inhaler use, even if they interact for just 10 minutes or if the patient reports data only a few days in the month.
At-a-Glance: Current vs. Proposed RPM/RTM Billing Rules
| Billing Aspect | Current (2025) | Proposed 2026 |
| RPM Device Supply & Data | ≥16 days of patient data required per month to bill RPM device code (99454). No billing if <16 days. | ≥16 days stays under 99454; new code 99XX4 for 2–15 days of data (min 2 days) – pays same as 99454. |
| RPM Care Management Time | ≥20 minutes of clinical staff/MD time per month required for first RPM service code (99457). No billing if time <20 min. | ≥20 min stays for 99457; new code 99XX5 for 10–19 minutes of RPM management time, reimbursed at ~50% of 99457. Allows billing for shorter care interactions. |
| RTM (Therapeutic) Device Data | ≥16 days of data required for RTM device codes (e.g. 98976 for respiratory, 98977 for musculoskeletal). No billing if <16 days. | New RTM codes 98XX4, 98XX5 for 2–15 days of data (min 2 days) in musculoskeletal and respiratory monitoring. Existing 98976/98977 for ≥16 days remain. |
| RTM Care Management Time | ≥20 minutes per month required for RTM management (98980 initial) to bill. No code for <20 min. | New RTM code 98XX7 covers 10–19 min of RTM management time1. 98980 would apply for ≥20 min as before. |
What’s NOT changing
No new device code was added for certain niches like Cognitive Behavioral Therapy digital monitoring (CMS left those to be handled by local contractors). Also, the requirement for “interactive communication” with the patient each month still applies for billing RPM/RTM service codes – meaning a live call or similar interaction is needed at least once per month for the service codes (both the new and existing ones).
How These Changes Create Value for Providers
For healthcare providers using Virtual Care platforms such as CareSimple, these proposed changes can significantly enhance both the reach and the financial viability of RPM programs:
1. More Patients Eligible & Engaged
By dropping the 16-day rule to a 2-day minimum, providers can enroll patients in RPM who previously wouldn’t qualify or were considered “too risky” to justify the effort 1. Examples include patients with shorter-term needs (like a 1-week blood pressure check post-surgery) or those who tend to be forgetful with devices. Now, even limited data can be billed, so clinicians can offer RPM more broadly without fear of not being reimbursed. This widens the patient base for remote monitoring, extending its benefits to populations like post-acute care and those with intermittent monitoring needs.
2. Reduced Uncompensated Care (Fewer Billing Gaps)
Under current rules, if a patient didn’t hit 16 days of use or if staff spent 15 minutes instead of 20, the practice got $0 for that month. Those gaps are frustrating and costly. The new codes ensure partial work still pays. Providers will see far fewer months of unpaid RPM services, as even minimal compliance (a couple of readings, or a quick call) yields some reimbursement. This smooths out revenue flow and makes monthly RPM income more predictable. In short, RPM programs become more financially resilient, with less revenue “leakage” due to technicalities.
3. Higher ROI and Program Sustainability
With the ability to bill incrementally, the return on investment for RPM technology improves. Clinics can start patients on RPM without needing a guarantee of perfect adherence. If a patient only engages half as much one month, that month isn’t a total loss financially. Over a large population, these incremental payments add up, helping offset the costs of devices and staff time. This should encourage more providers to invest in RPM programs (or expand existing ones) since the risk of not getting paid is lower. In turn, CareSimple may see increased adoption of its platform as providers justify expansion with this friendlier reimbursement structure.
4. Emphasis on Timely Care vs. Time Counting
Clinicians can now focus on delivering timely interventions without worrying about hitting a 20-minute quota. The new 10-minute code rewards quick responses to patient needs. For example, if an RPM alert comes in about rising blood glucose, a nurse’s fast 10-minute follow-up call can be billed immediately via 99XX5, rather than delaying help or bundling multiple issues into one larger call. This fosters better care quality – patients get attention when they need it, and providers know even those small touches count. It aligns financial incentives with proactive care: do the right thing at the right time, and you’ll be paid for it. Additionally, staff productivity can improve as they can break their workflow into shorter tasks and still capture revenue for each task.
5. New Service Offerings (Therapeutic Monitoring)
The expansion of RTM codes means CareSimple customers might branch out beyond physiologic monitoring. For instance, a primary care clinic could use the CareSimple platform (or an integrated solution) to support a physical therapy program remotely. With new RTM billing available, they could partner with physical or respiratory therapists to monitor patients’ exercise adherence or inhaler usage via simple apps or devices, billing Medicare for those services. It opens doors to integrated care models – e.g., managing a patient’s hypertension with RPM while also managing their COPD with RTM – all reimbursable.
6. Alignment with Value-Based Care Goals
These changes reinforce Medicare’s move toward continuous, home-based care management, which is very much in line with broader healthcare trends. CMS explicitly views RPM as a “longitudinal service, not a short-term episode” — providers can keep a patient on RPM as long as needed for chronic disease management 2. For CareSimple customers in value-based payment models, this is great news: it means they can more easily maintain chronic patients under monitoring indefinitely, improving long-term outcomes (e.g., blood pressure control, as studies suggest) 2. More flexible RPM billing supports preventative care and early intervention, which lead to better patient outcomes and potentially shared savings or quality bonuses for providers. In summary, the rule changes don’t just improve billing – they encourage the kind of sustained patient engagement that value-based care programs are looking for.
Compliance and Oversight: Persistent Issues with New Codes
While the proposed rule is largely positive for remote care programs, Providers should be mindful of compliance as the landscape shifts:
Risk of Overutilization & Scrutiny
CMS has noted that allowing billing with as few as 2 days of data or 10 minutes of time could be ripe for abuse by bad actors 1. For example, an unscrupulous provider might enroll patients, barely monitor them (just 2 readings), and still bill Medicare. Regulators are on alert: a 2024 HHS Office of Inspector General (OIG) report already raised concerns about RPM overuse and improper billing practices 1. Therefore, we should expect increased auditing and enforcement in RPM/RTM. Providers using these new codes must use them appropriately – documenting medical necessity for short monitoring stints and ensuring that even if only 2-15 days of data were collected, it was reasonable for the patient’s condition. Similarly, time logs for the new 10-minute code should clearly show clinical engagement (and the required patient interaction) took place.
Continued Requirements
It’s important to note that all existing RPM program rules still apply aside from the adjusted thresholds. Providers must obtain patient consent for RPM each year, use a reliable device that automatically uploads data, and have a live interactive contact each month when billing management codes 1. None of these foundational compliance rules changed. So CareSimple customers should continue to follow best practices (which CareSimple’s platform can help facilitate, e.g. by logging time spent, tracking data days, and prompting monthly calls).
Prepare Internally
Now is a good time for organizations to update their RPM protocols and training. Billing teams will need to plan for the addition of the new CPT codes if finalized (99XX4, 99XX5, etc.) and understand the scenarios for their use. Clinical staff should be educated that, for instance, if they only have a quick interaction, they should still log that time because it’s billable under the new rule. Documentation templates might be adjusted to capture the justification for using a short-duration code (e.g., “patient was on service only 10 days this month due to early hospitalization discharge”). By shoring up these processes, providers can confidently utilize the new flexibility without error.
Watch for Final Rule Nuances
Remember, this is a proposed rule. Details could change in the final rule (expected by November 2025). For example, CMS will finalize the exact reimbursement rates for these codes and any additional guardrails. The agency has solicited feedback on whether RPM and RTM services should be valued the same given similar workflows, and whether to use outpatient cost data to set device code pricing (which could affect reimbursement levels) 1. CareSimple customers should stay tuned for the final rulings on these questions. Any significant changes will need to be accounted for in 2026 planning (for instance, if the device code payment is adjusted). We will likely provide an update once the final rule is published so that everyone knows the confirmed facts.
Next Steps and Action Items
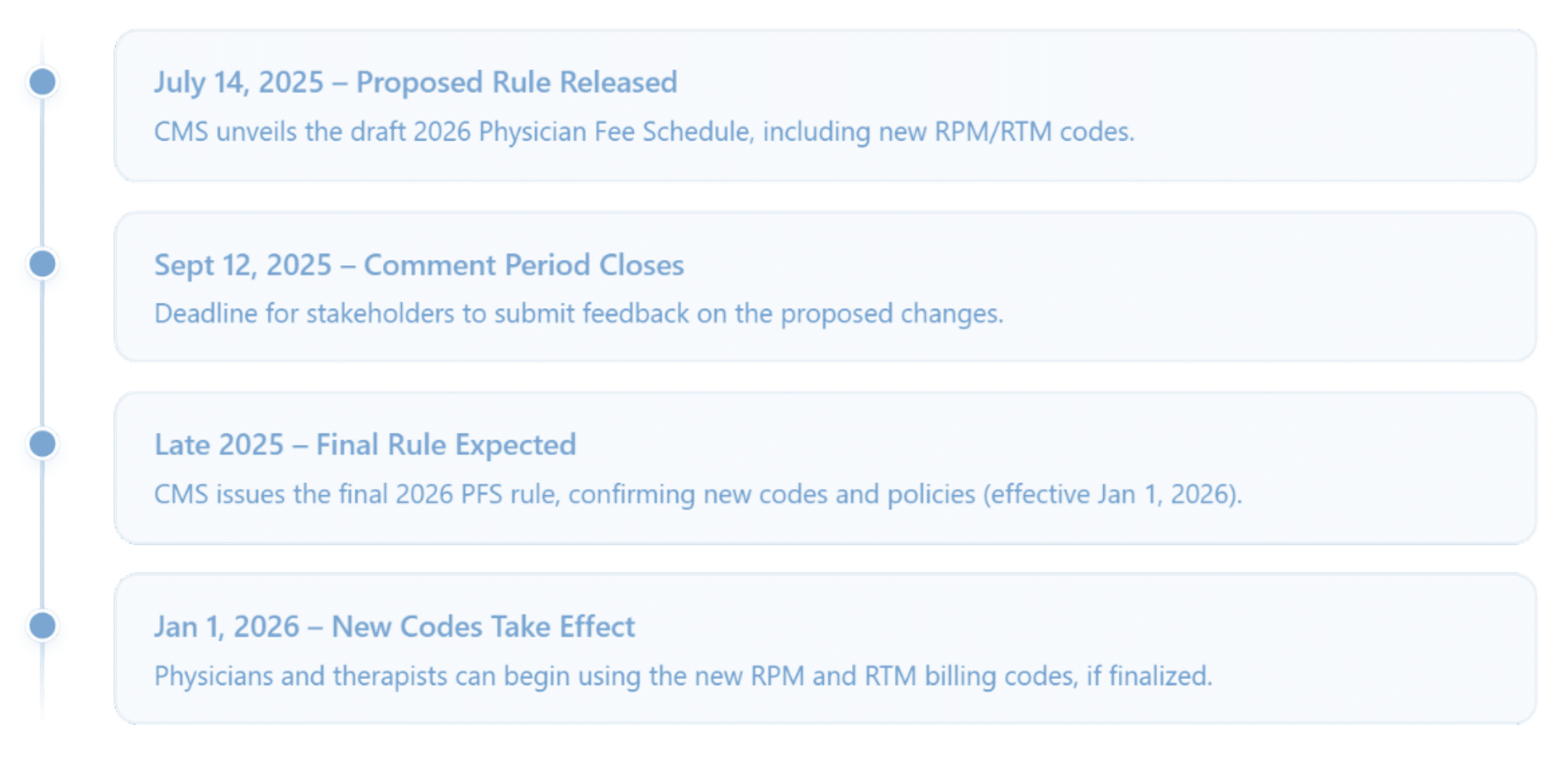
Public Comment Period (Summer 2025)
CMS is inviting stakeholders to comment on the proposed changes before they are finalized 1. The comment period runs until September 12, 2025. Providers can take this opportunity to voice support for these RPM enhancements and share any data or stories that reinforce their value (or concerns to watch out for). The Nixon Law Group suggests that comments with real-world evidence (e.g. how 5 days of monitoring prevented a hospitalization) can be very impactful 1. As stakeholders in remote monitoring, all providers involved in RPM and/or RTM should do so, to help ensure the final policy is as favorable and clear as possible.
| POSTING YOUR COMMENTS BEFORE SEPTEMBER 12TH 2025 |
| https://www.regulations.gov/document/CMS-2025-0304-0009 |
Implementation Planning
Assuming these proposals are adopted, they would take effect January 1, 2026 2. CareSimple customers should begin preparing to implement the new codes:
- Update billing software and EHR templates with CPT 99XX4, 99XX5, 98XX4, 98XX5, 98XX7 and their descriptors.
- Train clinical staff and coding teams in Q4 2025 about the new billing criteria.
- Identify which patient populations would immediately benefit. For example, identify current RPM patients who sometimes fall short of 16 days or 20 minutes – they represent quick wins where revenue can be recaptured once the rule is in effect.
- Adjust patient onboarding criteria – you may start enrolling patients in late 2025 that previously you wouldn’t have (knowing the new codes will cover them in 2026)
Timeline
Conclusion
The 2026 Medicare PFS proposal is a game-changer for remote monitoring. It lowers the hurdles that previously limited RPM’s use, making it easier for providers to extend digital care to more patients and get paid for doing so. For CareSimple customers and other providers, this means greater utilization of RPM services, improved revenue capture, and the ability to innovate new remote care offerings around these flexible reimbursement options. If adopted, these changes will empower care teams to focus on what matters – the patient’s health – with fewer arbitrary billing rules getting in the way. At the same time, providers should proceed responsibly, upholding high compliance standards to ensure that this new latitude is used to deliver genuine clinical value. By preparing now and staying engaged in the rulemaking process, CareSimple and its clients can fully capitalize on the opportunities of the 2026 fee schedule, positioning their RPM programs for success in the years ahead.
If adopted, these changes will empower care teams to focus on what matters – the patient’s health – with fewer arbitrary billing rules getting in the way.
CMS.GOV